In the quest for relief from arthritis, many people wonder if it is possible to clean out the condition from their joints. This article explores the question of whether arthritis can be eliminated and offers insights into the potential methods and treatments that can provide a sense of cleaning out or alleviating the symptoms. While finding a complete cure for arthritis may still be elusive, there are various strategies and approaches that can help manage the condition and improve joint function.
What is Arthritis?
Arthritis is a common chronic condition that affects millions of people worldwide. It refers to the inflammation of one or more joints, resulting in pain, stiffness, and decreased mobility. Arthritis can affect people of all ages and commonly occurs in older adults. It is important to understand the different types, causes, and symptoms of arthritis in order to effectively manage and treat the condition.
Definition
Arthritis is a broad term that encompasses over 100 different rheumatic diseases and conditions. The most common forms of arthritis include osteoarthritis (OA), rheumatoid arthritis (RA), and psoriatic arthritis. While each type of arthritis has unique characteristics, they all share the common feature of joint inflammation.
Types of Arthritis
- Osteoarthritis (OA) – This is the most prevalent form of arthritis, often referred to as “wear and tear” arthritis. It occurs when the protective cartilage that cushions the ends of bones wears down over time, leading to joint pain and stiffness.
- Rheumatoid Arthritis (RA) – RA is an autoimmune disease that causes chronic inflammation of the joints. It primarily affects the lining of the joints, resulting in pain, swelling, and deformity.
- Psoriatic Arthritis – This type of arthritis develops in individuals with psoriasis, a skin condition characterized by red, scaly patches. Psoriatic arthritis can cause joint pain, stiffness, and swelling, typically affecting the toes, fingers, lower back, and knees.
Causes and Symptoms
The causes of arthritis vary depending on the type. Osteoarthritis is often associated with aging, joint injury, obesity, and genetics. Rheumatoid arthritis, on the other hand, is an autoimmune disease where the body’s immune system mistakenly attacks its own tissues. Psoriatic arthritis is believed to be a combination of genetic and environmental factors.
Regardless of the type, common symptoms of arthritis include joint pain, swelling, stiffness, and decreased range of motion. In addition to these physical symptoms, arthritis can also have a significant impact on a person’s emotional well-being, causing frustration, anxiety, and depression.
Current Treatments for Arthritis
While there is no cure for arthritis, several treatment options are available to manage the symptoms and improve joint function. These treatment approaches can be categorized into three main categories: medications, physical therapy, and surgical options.
Medications
Medications play a crucial role in the management of arthritis symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used to relieve pain and reduce inflammation. For more severe cases, disease-modifying antirheumatic drugs (DMARDs) or biologic agents may be prescribed to slow down the progression of the disease and prevent joint damage.
Physical Therapy
Physical therapy is a non-invasive approach to arthritis management that aims to restore joint function, strengthen muscles, and improve mobility. Therapeutic exercises, manual therapy techniques, and modalities such as heat and cold therapy may be employed to reduce pain and increase joint flexibility.
Surgical Options
In cases where conservative treatments are ineffective, surgical interventions may be considered. Joint replacement surgery, such as total knee or hip replacement, is a common surgical option for individuals with severe arthritis-related joint damage. This procedure involves replacing the damaged joint with an artificial implant, providing pain relief and improved mobility.
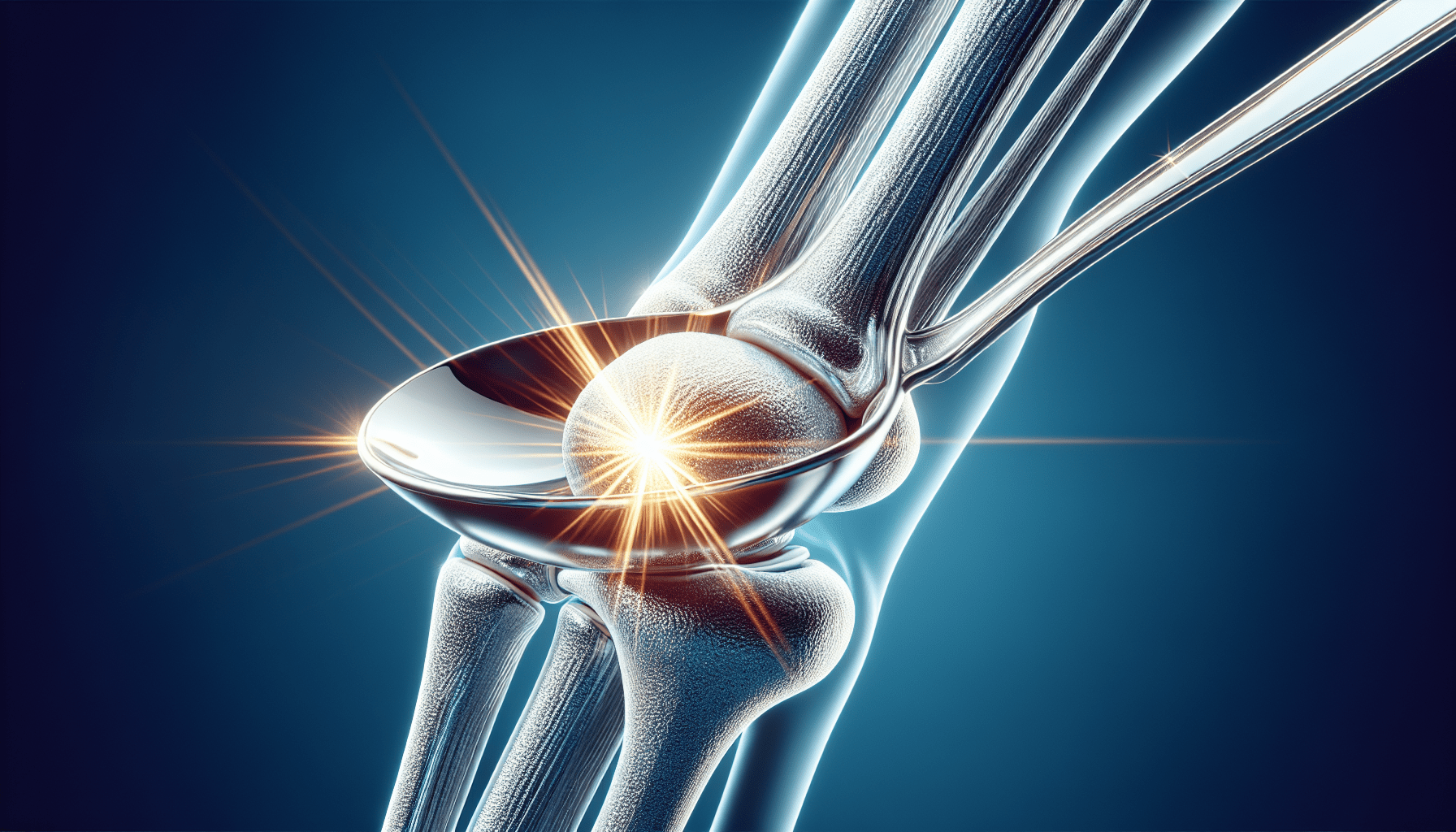
Joint Cleaning Procedures
Joint cleaning procedures, also known as joint debridement or joint lavage, are minimally invasive techniques used to remove damaged or inflamed tissue from the joint. This can help alleviate pain, reduce inflammation, and improve joint function. Three common joint cleaning procedures include arthroscopy, synovectomy, and joint lavage.
Arthroscopy
Arthroscopy is a minimally invasive surgical procedure that allows healthcare professionals to visualize, diagnose, and treat joint conditions using a small camera called an arthroscope. During the procedure, small incisions are made, and the arthroscope is inserted into the joint. This allows the surgeon to examine the joint structures and remove any damaged tissue, bone fragments, or loose cartilage.
Synovectomy
A synovectomy is a surgical procedure that involves the removal of the synovial membrane, the tissue lining the joint. This procedure is commonly performed in cases of rheumatoid arthritis, where the synovium becomes inflamed and thickened, causing pain and joint damage. By removing the inflamed tissue, synovectomy can help alleviate pain and potentially slow down disease progression.
Joint Lavage
Joint lavage, also known as joint irrigation, involves flushing the joint with a sterile fluid to remove debris, inflammatory cells, and other irritants from the joint space. This procedure can be performed using a needle and syringe or during arthroscopy. Joint lavage aims to reduce inflammation, relieve pain, and improve joint function.
1. Arthroscopy
Definition and Procedure
Arthroscopy is a minimally invasive surgical procedure used to visualize and treat joint conditions. It involves inserting a small camera called an arthroscope into the joint through small incisions. The arthroscope provides a clear view of the joint structures, allowing the surgeon to diagnose and address any abnormalities or damage.
During the procedure, the surgeon may use specialized tools to remove damaged tissue, bone fragments, or loose cartilage. They can also repair torn ligaments or remove inflamed synovium if necessary. Arthroscopy is commonly performed on joints such as the knee, shoulder, hip, and ankle.
Benefits and Risks
Arthroscopy offers several benefits compared to open surgery. The small incisions result in minimal scarring, reduced pain, and faster recovery times. By addressing joint conditions early on, arthroscopy can potentially prevent further joint damage and delay the need for more invasive procedures like joint replacement surgery.
As with any surgical procedure, arthroscopy carries certain risks. Infection, bleeding, blood clots, and damage to surrounding structures are possible complications. However, these risks are relatively low compared to open surgery.
Patient Recovery
When undergoing arthroscopy, patients typically experience a shorter recovery period compared to traditional open surgery. Following the procedure, pain and swelling in the joint are common but can usually be managed with pain medications and ice packs. Physical therapy may be recommended to restore joint mobility and strength. Most patients can resume their normal activities within a few weeks, although strenuous activities may need to be avoided for a longer period.
2. Synovectomy
Definition and Procedure
Synovectomy is a surgical procedure that involves the removal of the synovial membrane, which lines the joint. It is typically performed in cases of rheumatoid arthritis, where the synovium becomes inflamed and thickened, leading to pain and joint damage.
During the procedure, the surgeon makes a small incision and removes the inflamed synovial tissue either partially or completely. This can be done using traditional open surgery or minimally invasive techniques such as arthroscopy. Synovectomy is most commonly performed on larger joints such as the knee, wrist, and ankle.
Benefits and Risks
Synovectomy provides several benefits for individuals with rheumatoid arthritis. By removing the inflamed synovium, synovectomy can help relieve pain, reduce joint swelling, and potentially slow down disease progression. It may also improve joint function and increase the effectiveness of other arthritis treatments.
Although synovectomy is generally considered safe, there are potential risks and complications. Infection, bleeding, and damage to nearby structures are possible. Additionally, synovectomy may not be suitable for everyone, depending on the extent of joint damage and individual health factors.
Patient Recovery
Recovery following synovectomy depends on factors such as the joint involved, surgical technique, and individual healing capabilities. Some pain and swelling are expected post-surgery, but these can be managed with pain medications and ice packs. Physical therapy may be recommended to ensure proper joint rehabilitation and prevent stiffness. It is important for patients to follow the surgeon’s instructions and attend follow-up appointments for optimal recovery.
3. Joint Lavage
Definition and Procedure
Joint lavage, also known as joint irrigation, involves cleansing the joint by flushing it with a sterile fluid. This procedure aims to remove debris, inflammatory cells, and other irritants from the joint space, reducing inflammation and improving joint function. Joint lavage can be performed using a needle and syringe or as a part of arthroscopy.
During the procedure, the surgeon inserts a needle into the joint space and injects a sterile solution, such as saline or lactated Ringer’s solution. The fluid is then flushed through the joint, carrying away any unwanted substances. Joint lavage can be beneficial for individuals with joint pain and swelling caused by arthritis or other joint conditions.
Benefits and Risks
Joint lavage can provide short-term relief of symptoms for individuals with arthritis. By removing irritants from the joint space, it can reduce inflammation, alleviate pain, and potentially improve joint mobility. However, the long-term benefits of joint lavage are still a subject of debate in the medical community.
As with any medical procedure, there are risks associated with joint lavage. Infection, bleeding, and damage to surrounding structures are potential complications. It is crucial for the procedure to be performed by an experienced healthcare professional to minimize these risks.
Patient Recovery
Recovery following joint lavage is typically swift, with minimal downtime. Some discomfort and swelling are normal immediately after the procedure, but these symptoms usually subside within a few days. Pain medications and ice packs may be recommended to manage any post-procedure discomfort. Physical therapy and maintaining a healthy joint care routine can help optimize recovery and maintain joint health in the long term.